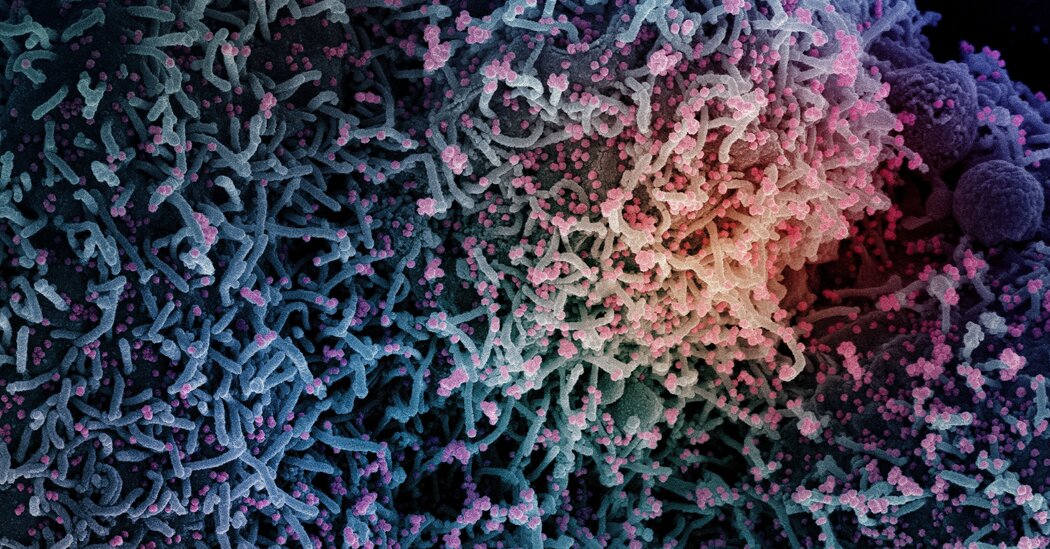
Because an immunocompromised host doesn’t produce a lot of antibodies, many viruses are left to propagate. And new mutant viruses that resist the antibodies can multiply.
A mutation that allows a virus to evade antibodies isn’t necessarily advantageous. It could make the virus’s spike protein unstable so that it can’t latch quickly onto a cell, for example. But inside someone with a weak immune system, viruses may be able to gain a new mutation that stabilizes the spike again.
Similar mutations could have built upon themselves again and again in the same person, Dr. Pond speculates, until Omicron evolved a spike protein with just the right combination of mutations to allow it to spread supremely well among healthy people.
“It certainly seems plausible,” said Sarah Otto, an evolutionary biologist at the University of British Columbia who was not involved in the study. But she said scientists still needed to run experiments to rule out alternative explanations.
It’s possible, for example, that the 13 spike mutations offer no benefit to Omicron at all. Instead, some of the other spike mutations could be making Omicron successful, and the 13 are just along for the ride.
“I would be cautious about interpreting the data to indicate that all of these previously deleterious mutations have been adaptively favored,” Dr. Otto said.
Dr. Pond also acknowledged that his hypothesis still has some big gaps. For example, it’s not clear why, during a chronic infection, Omicron would have gained an advantage from its new “bubble” method for getting into cells.
“We just lack imagination,” Dr. Pond said.
James Lloyd-Smith, a disease ecologist at U.C.L.A. who was not involved in the study, said that the research revealed just how hard it is to reconstruct the evolution of a virus, even one that arose recently. “Nature is certainly doing its part to keep us humble,” he said.